COVID and the loss of smell
Normally, one-star reviews of products are rarely cause for alarm. People love to complain to whoever will listen, even if it means typing into the void of the internet.
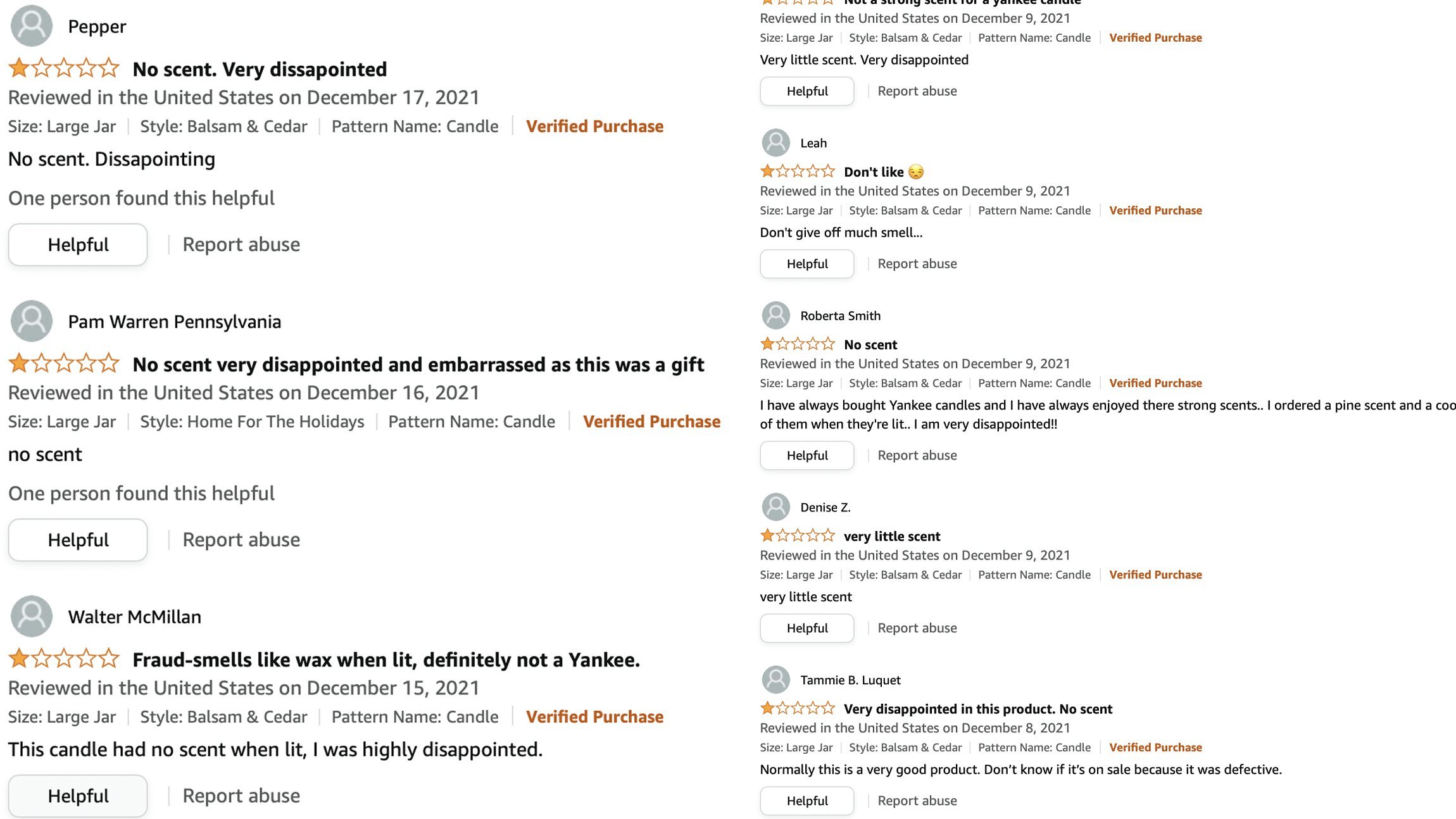
But knowing what we know about the correlation between COVID infection and anosmia, the lack of smell, this uptick in negative reviews of Yankee Candle products might raise an eyebrow:
With the Omicron variant making its rounds right before the 2021 candle-giving season, some people are apparently starting to experience a novel olfactory sensory loss, one of the most predictive symptoms of COVID.
Outside of the pandemic, a loss of smell is not often thought of as being too clinically significant. The common cold with all the accompanying stuffiness and nasal blockage produces loss of smell. A head injury that leads to shearing of the olfactory nerves leads to anosmia, but treating that loss of sensation is secondary to treating the, you know, possible concussion. Exposure to environmental factors can also dampen the sense of smell, brought on by smoking or allergens, but the loss of smell is not usually a new experience for these people.
So what is the reason behind this loss of smell?
Obviously, the science of SARS-CoV-2 is a new and developing situation, with much more research time and energy being devoted to answering these questions than just 3 years ago. However, there are a few things that have been discovered so far that may explain anosmia.
The angiotensin converting-enzyme 2 (ACE2) receptor is expressed on the cell surface, and has been implicated as the “entryway” by which the SARS-CoV-2 virus particle gains access to cells. ACE2 is expressed widely across the respiratory epithelium, which explains why these cell types are particularly vulnerable. ACE2 is also found throughout the body, such as in the cells of the heart, blood vessels, gallbladder, and male reproductive cells among others. 1
ACE2 is also expressed, as you might expect, in cells of the olfactory epithelium, the tissue found at the back of the nasal cavity. Embedded within the olfactory epithelium are olfactory receptor neurons (ORNs), the cells that respond to molecules floating in the air that we breathe. Activity at these neurons in different combinations leads to our perception of smells.
https://indianexpress.com/article/explained/why-do-some-covid-19-patients-lose-their-sense-of-smell-6430325/
You might be surprised to learn, as I was, that ACE2 is not actually expressed on these ORNs. Instead, ACE2 is found on another population of cells in the olfactory epithelium, the sustentacular cells. 2 These cells have also been called the support cells of the olfactory system. They are closely associated with the ORNs, sometimes wrapping around them. They perform functions akin to glial cells in other parts of the nervous system, such as destroying and clearing away of dead ORNs or other foreign particles (phagocytosis) and providing a secondary source of glucose, the molecule that functions as a source of cellular energy.
A leading theory suggests that after the virus infects the sustentacular cells, it triggers the onset of a local inflammatory cascade. This causes these support cells to now behave in unexpected ways, possibly preventing them from working the way they should in a healthy, uninfected person.
A related theory suggests that systemic inflammation is to blame. In this framework, the presence of the virus in the epithelium causes infiltration of systemic immune cells, which go on to release various pro-inflammatory cytokines. 3
Smell and taste are two chemical senses that are closely related. Ageusia, the loss of taste, therefore can also be affected by COVID. In line with the above theories, and according to one study, the ACE2 receptor is also found on certain populations of cells in taste buds. 4
While much work has yet to be done in the field, the recommendation still stands: prevention is more important than treatment.